
Second, I would contend that we are still in the early phase of a Copernican revolution in healthcare in which healthcare providers revolve around the patient rather than the reverse situation that has been the case since the advent of the modern hospital. However there has been a huge proliferation of “Pay for Performance (P4P)” projects over the past decade that are linked to process of care and intermediate outcomes, such as blood pressure control, although there is also a large critical literature of P4P.

Indeed, Kindig set out an ambitious proposal for such an approach in the 1990s, but I have not seen any uptake as yet ( 13). Where are these developments taking us? I am convinced that ultimately health systems will remunerate providers based on improvements in outcome and not so much on volumes or processes of care. have recently proposed how Health Adjusted Life Expectancy can be applied in clinical settings ( 12). There has also been considerable research on the application of such indicators for the development of composite measures of population health status, that has gained significant traction since the 1993 World Development Report, which popularized the concept of Disability Adjusted Life Years ( 11). Research is underway to assess the applicability of PROMs to chronic conditions such as chronic obstructive pulmonary disease and diabetes ( 10). Since 2009, the English National Health Service (NHS) has mandated the pre- and post-operative collection of PROMs data for four procedures including hip and knee replacement, varicose vein surgery and groin hernia surgery, and the results are regularly reported ( 9). While many of the original applications were in health economics, such as studies to establish cost-effectiveness measures, they are now being rebranded as Patient-Reported Outcome Measures (PROMs). A key contribution has been the development of relatively short indices that capture dimensions of physician and emotional health, such as the 36-item Short-Form Health Survey, and the 15-item Euroqol 5-D, which have now been studied in many populations ( 7, 8). In his 1966 classic, Donabedian identified five challenging aspects of using outcomes to measure the quality of care:Īside from survival/death other more subjective measures such as patient attitudes, satisfaction, and disability/rehabilitation are more difficult to measure ( 6).Īlthough these considerations continue to apply almost 50 years later, great strides have been made in measuring individual and population health status. To this day, the quality field continues to be preoccupied with intermediate outcomes of the processes of care that have implications for patient safety. Forest, I too would pay homage to Donabedian, specifically to his 1966 paper in which he set out the structure, process and outcome framework for assessing the quality of care ( 6). Although it had early origins such as Florence Nightingale’s efforts to record outcomes during the Crimean War in the 1850s, and Ernest Codman’s work on the “end results” of medical care in the early 1900s, a focus on outcomes has been slow to come about ( 4, 5). The first of these is the development of an outcome focus on healthcare.

I would like to add, however, that over the past few decades we have arrived at two fundamental changes in the way that we approach health and healthcare that will also have significant implications for health policy.
#Dr gridlock driver
1 increased more between 20 than it did in the previous 12 years, which suggests that this could beĪ major cost driver in the years ahead ( 3). Moreover, the Organization for EconomicĬooperation and Development (OECD) has reported that income inequality have estimated to have accounted for 20% of healthcare costs in theĮuropean Union in 2004 ( 2). Will bring about a revolution in health policy ( 1), and I would notĬhallenge any of them, although I would emphasize the importance of tackling socio-economic health inequalities,
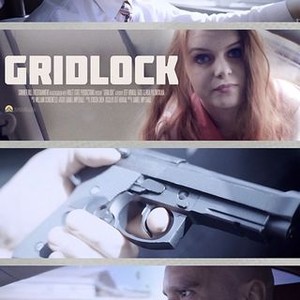
Forest has made a compelling case for five advances in health research that “Gridlock” is a term that has been applied to the state of health policy in Canada and the United States for


 0 kommentar(er)
0 kommentar(er)
